
Revenue Cycle Management
Our multi-layered, deeply integrative approach incorporates predictive analytics, machine learning, and comprehensive root-cause analysis to prioritize and address unpaid claims. Clover has managed over $8 billion in client accounts receivable, and achieved cash recovery totaling $2.1 billion through our Revenue Cycle Management solutions.

Enrollment, Billing, and Claims
Clover redefines claims management for payers with insightful, end-to-end solutions. We have more than 23 years of experience handling claims of all complexities across all products and over 20 claims platforms. Our experience in plan build and benefit configuration across multiple products brings our all-round expertise to ensure higher claims processing accuracy. In addition, we manage enrollment and billing operations across multiple plan types. Our transformational solutions allow for optimizing efficiency, reducing inaccuracies, boosting timeliness, and enhancing member and provider satisfaction.

Clinical Services
By integrating technology-driven clinical denial management and virtual nurse/telehealth services, we optimize processes using Payer-Provider synergy, AI automation, and global nursing expertise. This fosters efficient denial resolutions, precise coding, real-time analytics, and enhanced patient-provider interactions. With our team and adept healthcare professionals, we deliver improved outcomes, reduce health disparities, afford better care access, and a more effective healthcare system.

Provider Network Operations
Today’s payers are demanding a solution for the costly, high-stakes problem of unreliable provider data. Clover addresses the issue head-on, turning the tide on member dissatisfaction, provider friction, administrative overhead, and regulatory penalties. Our solutions address key requirements of the No Surprises Act.
With Clovers Provider Forward™ platform, you will experience a holistic view of the provider journey and high-leverage touch points across recruiting, contracting, credentialing and data maintenance processes. It effortlessly improves the overall Provider Network Operations efficiency by over 35% with automation and intelligence

Engagement Services
clover makes it easy for members and providers to achieve a higher resolution through specialized talent combined with end-to-end Contact Center as a Service solutions, including speech analytics and omnichannel platforms. Our primary goal is to enhance both member and provider experiences by offering solutions that streamline customer engagement and foster a robust healthcare network. By prioritizing customer-centricity, we improve Net Promoter Scores (NPS) and enhance healthcare outcomes.

Payment Integrity
Clovers solutions streamline claims payment processes, eliminating fragmented and disjointed procedures that often lead to payment inaccuracies. We look at each claim with a holistic approach, prioritizing our analysis based on the highest recoverable payment amounts. Our payment integrity solution is built with an innovative 360-degree view of claims assessment. These solutions include Data Mining and Claims Repricing, as well as Clinical Audits, working in tandem to create value in both pre and post-pay instances.

Patient Engagement
Maintaining excellent customer service is a crucial aspect of a provider’s long list of responsibilities, particularly in the healthcare industry. Clover offers a distinct approach to customer service that transforms the provider-patient relationship.
We serve as an extension of your practice, helping improve your ability to provide better quality of care, patient outcomes and satisfaction, while ensuring strong financial performance. Our patient engagement solutions cover diverse services like appointment setting, patient billing and collections, as well as omnichannel communication support. Clover strives for a comprehensive patient engagement strategy that benefits both providers and patients.
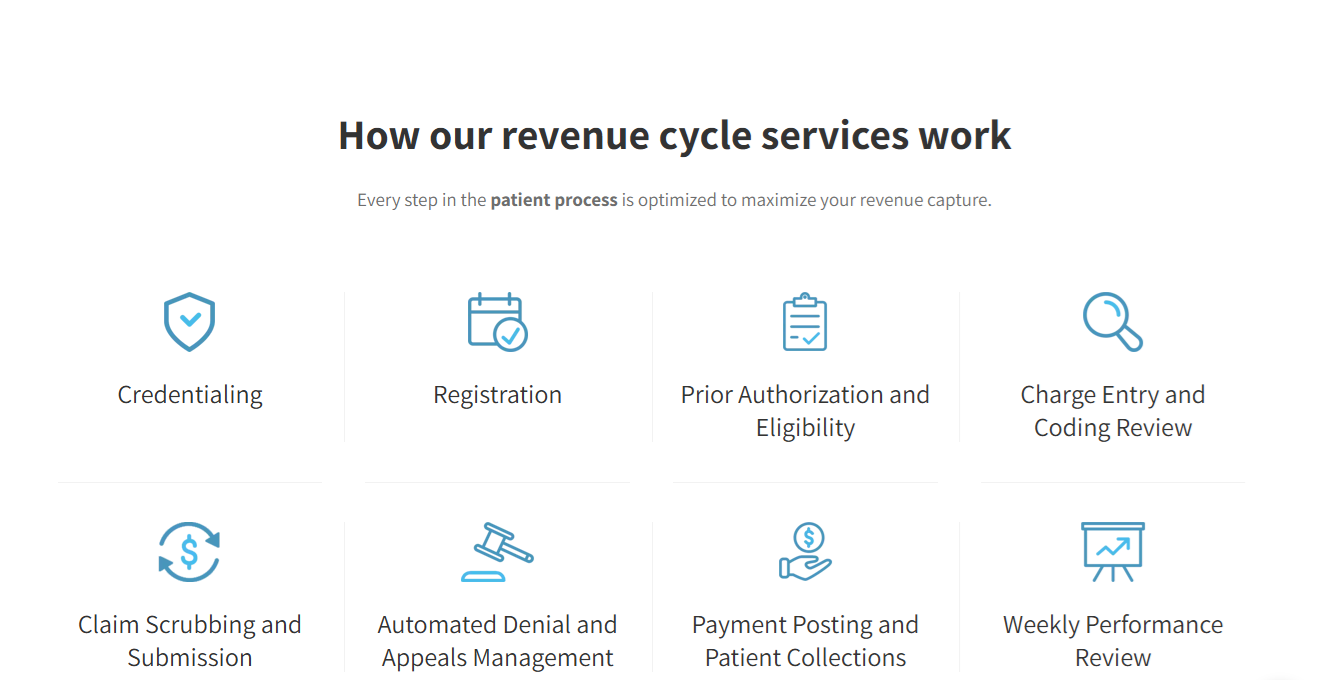
Patient Access
To cover all aspects of patient access, Clover employs a comprehensive process that ultimately improves the patient experience. We prioritize insurance verification, benefit confirmation, authorization, and referrals to aid providers in improving their patient access quality. In an industry marked by inefficiencies, our approach addresses financial clearance intricacies, helping clients maximize their potential reimbursements.
From In-House to Outsourced RCM: Everything You Need to Know
The thought of moving to RCM for healthcare providers, doctors, practice owners, laboratorians, and other stakeholders can be considerable. So, we created this eBook to cover some of the common concerns when considering a revenue cycle management service collaboration, as well as:
- Benefits of Switching to an RCM Service
- Reasons for Outsourcing
- Factors in the Decision Making Process for a healthcare provider
- Ongoing Learning to Make the Most of Outsourced RCM Services
- Revenue Cycle Management Step-By-Step
- 10 FAQs About RCM Services Revenue Cycle Management
Speak with an expert to hear more
Connect with a Clover expert today. Let’s explore innovative solutions tailored to your organization’s unique needs.
Contact Us

